Scientists have spotted a small set of easily overlooked brain cells that is activated during persistent pain — the kind that lasts long after an initial injury. The research was performed in mice, but if it can be confirmed in humans, the work could lead to new therapies for chronic pain.
Such pain affects roughly one in five people worldwide. “Pain is in your head. But it is very real,” says Nicholas Betley, a biologist at the University of Pennsylvania in Philadelphia and a co-author of a new study describing the findings.
The authors’ experiments also show that the release of a specific signalling chemical in the brain can dampen the activity of the persistent-pain neurons, suggesting that the brain itself has an innate pain-killing mechanism.
In the study, published in Nature1 on 8 October, Betley and his team focused on a brain region called the parabrachial nucleus, which receives multiple types of sensory information from the body. The nucleus then relays those data to other regions of the brain.
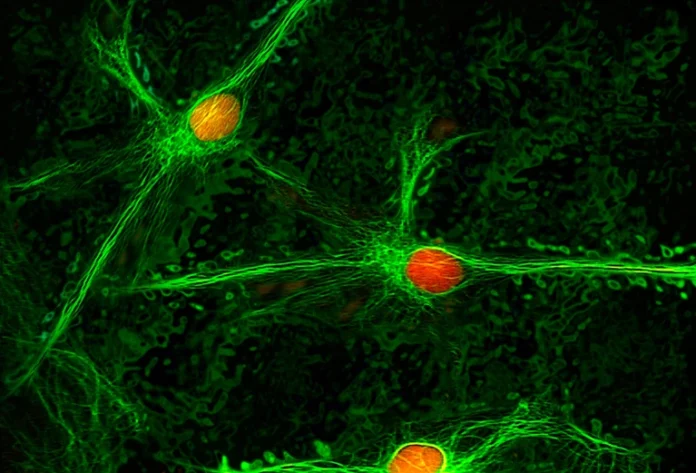
In studies on mice, the researchers identified a subset of neurons distributed throughout the parabrachial nucleus that switched on after an initial painful stimulus, such as a cut to a nerve, and remained active long after the insult. The persistent-pain neurons carry receptors for a signalling molecule called neuropeptide Y.
When the researchers artificially activated these ‘Y1R’ neurons, mice showed pain-associated behaviours. When the scientists blocked the activity of these neurons, the animals’ persistent pain decreased, yet they had normal short-lived pain responses after being exposed to dangers, such as touching a hot surface. The Y1R neurons alone don’t cause the feeling of pain, Betley says. But, they form part of the network “that leads to the sensation that we refer to as pain”.
Mice with persistent pain were also deprived of food or water or exposed to a frightening stimulus, such as a component of bobcat urine. In each case, the animals’ behaviour and neural activity suggested that their persistent pain had been reduced. For example, two weeks after a nerve injury, hungry mice ignored a poke to their paws that would normally make them recoil. “In the wild, we think this would allow them to shift focus from their pain to go out and seek food,” says Betley.
The researchers attributed the pain reduction to an influx into the parabrachial nucleus of neuropeptide Y, which had been released by neurons in other parts of the brain that became active when the mice developed urgent needs. “Something more important than pain came along,” says co-author Ann Kennedy, a neuroscientist at the Scripps Research Institute in La Jolla, California. “We think of pain as just a sensory input … but the sensation of pain is a lot more malleable, and it’s changed by our experiences.”
The study makes a surprising, yet strong, case that the parabrachial nucleus is the site for crucial decision-making regarding pain and that neuropeptide Y is a key player, says Jeffrey Mogil, a neuroscientist at McGill University in Montreal, Canada. Still, he questions the assumption, used in this study and others, that assessing an animal’s behaviour just a few weeks after experiencing an injury is a good way to measure chronic pain. “Research over the last few years shows that things can change months after injury that maintain the pain,” he says.
Betley says that future work could explore whether calming strategies, such as meditation and acupuncture, might quiet persistent-pain neurons. Further research could also investigate neuropeptide-Y signalling as a new drug target — a potential breakthrough in a field in which progress has been elusive.
Although acute-pain mechanisms are relatively well understood, chronic pain remains much more mysterious. This has left people with limited treatment options. “Medications that are safe in the short term, like opioids, are not safe in the long term,” says Vivianne Tawfik, a neuroscientist at Stanford University School of Medicine in California.
The results might also lead to a measurable index of chronic pain. “You can’t ask an animal if they feel better. Now, we might be able to give the animal a treatment and see if the activity of these neurons goes down,” says Betley.